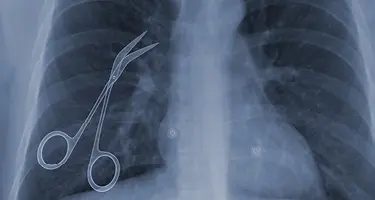
Across the country, a fresh wave of medical malpractice reform is reshaping the law. These bills and laws are part of a larger tort reform push sweeping through red and purple states, driven by business groups, insurers, and lawmakers eager to curb what they call “nuclear verdicts” and rein in litigation costs.
On one side, health care providers and hospitals argue they face crushing liability exposure, rising insurance premiums, and growing difficulty attracting and retaining physicians, especially in rural areas. Patient advocates warn that limiting damages and tightening legal standards risks shutting the courthouse doors on legitimate malpractice victims, shifting costs onto families and taxpayers.
Texas, Georgia, Utah, and South Carolina have emerged as national bellwethers in this fight. Each state is testing different legislative strategies—from capping medical damages and limiting noneconomic awards to restricting discovery and reshaping premises liability rules.
For lawyers and industry professionals, watching these four states offers a glimpse into where the next phase of U.S. malpractice reform is headed. Whether these measures ultimately deliver on their promises or fuel new legal challenges will shape the balance of patient rights and provider protections for years to come.
Texas: Reining in Big Verdicts and Tightening the Rules
Lawmakers and business groups in Texas frame the issue around “nuclear verdicts”—massive jury awards over $10 million that they argue inflate insurance premiums, scare off providers, and destabilize entire sectors. Whether these verdicts survive on appeal matters less politically than the narrative they fuel.
Senate Bill 30 (SB 30) rewires the evidence rules at the heart of malpractice cases. Plaintiffs can no longer present billed medical charges when those amounts vastly exceed what insurers or government payers actually reimburse. By forcing damages to reflect only amounts paid, the law sharply limits the headline numbers juries see. This not only reduces potential awards but reshapes the psychological framing of the case—smaller numbers, smaller emotional impact, smaller verdicts.
The law also narrows compensable harm definitions. Mental anguish must now reach a level of debilitation that substantially disrupts a person’s daily life. This raises the threshold for noneconomic damages, cutting off claims based on less severe emotional or psychological impacts. Critics warn this standard ignores the lived experiences of patients harmed by malpractice, but the legislative push prioritizes predictability and restraint over subjective harm.
Texas now requires disclosure of third-party litigation funding, forcing plaintiffs to reveal whether outside investors are bankrolling the lawsuit. This transparency is designed to discourage speculative lawsuits backed by litigation finance firms, which defense groups argue artificially inflate the volume and intensity of malpractice litigation. For health care providers, it reduces the risk of facing well-financed, high-stakes claims that would otherwise force expensive settlements.
Georgia: Anchoring, Procedural Barriers and Business-Driven Reform
Georgia’s tort reform package, driven by Senate Bills 68 and 69, represents one of the most sweeping overhauls in the country. The state’s political and business leadership has framed the push as essential to curbing what they describe as an abusive litigation environment, citing Georgia’s long-standing placement on the American Tort Reform Association’s “Judicial Hellhole” list. Behind the rhetoric, Georgia’s reforms reveal a calculated strategy: limit plaintiff tactics, impose procedural choke points, and deliver the insurance and business sectors the predictability they’ve demanded for years.
One of the most significant changes targets anchoring—the practice where plaintiffs’ attorneys suggest a high dollar figure for noneconomic damages like pain and suffering, hoping to set a reference point in the jury’s mind. Under the new law, attorneys must tie their damage arguments directly to evidence.
This ends the era of throwing out large, emotionally charged numbers disconnected from documented harm. Importantly, while Georgia hasn’t imposed a cap on damages, it has severely restricted the mechanisms plaintiffs use to elevate those numbers in front of juries.
Georgia has also reshaped the litigation timeline. The state’s reforms now impose automatic discovery stays when a motion to dismiss is filed. This forces plaintiffs to clear early legal hurdles before they can access the evidence needed to substantiate their claims—delivering defendants a powerful procedural advantage.
The law further shortens the window for plaintiffs to voluntarily dismiss and refile, cutting off strategies used to shift cases into more favorable venues or delay proceedings. Together, these procedural reforms act as a filter, thinning out claims before they can develop into full-fledged litigation.
Utah: Rural Provider Shortages and Targeted Malpractice Reforms
Instead of focusing solely on courtroom tactics or damage limitations, Utah has crafted reforms directly tied to a critical health care problem: rural provider shortages. House Bill 503 reflects a legislative response to one core question—how do you keep doctors practicing in areas where liability risk and insurance costs are driving them away?
At the heart of Utah’s reform is the recognition that malpractice exposure doesn’t just hit hospital systems; it hits small-town clinics and solo practitioners the hardest. Without the deep pockets or legal resources of larger providers, these practitioners often face premiums they simply cannot absorb.
HB 503 introduced minimum malpractice insurance requirements of $1 million, a move designed to standardize baseline coverage across the state and reduce insurer risk. Lawmakers framed this not as a burdensome mandate but as a stabilizing mechanism meant to keep insurance markets functional and available, particularly for small practices.
The law also introduces annual reporting requirements, tasking the Division of Professional Licensing with compiling detailed data on malpractice claims and outcomes. While framed as a transparency measure, this reporting structure lays the groundwork for future legislative action. With clear statewide data in hand, lawmakers can point to trends—real or perceived—to justify additional procedural restrictions or caps if current reforms fail to rein in costs.
South Carolina: Liability Shifts and the Road Toward Broader Reform
South Carolina’s recent malpractice reforms reflect an early-stage but consequential shift in how the state approaches liability—and they signal that broader procedural and systemic changes are likely ahead. Senate Bill 244 centers on one key adjustment: narrowing joint and several liability.
Under the previous rules, even a defendant found only marginally responsible—1% at fault—could be held liable for the entire damages award. This created a system where health care providers, particularly those with deeper pockets, became prime targets in lawsuits simply because they could pay.
SB 244 recalibrates this exposure by requiring juries to allocate fault across all responsible parties, even those not formally named in the suit. For health care providers, this represents meaningful relief, reducing the risk of being financially on the hook for damages disproportionate to their role in a case.
While the immediate reforms stop short of the procedural tightening seen in Texas or Georgia, South Carolina’s political signals point clearly toward future changes. Legislative leaders have framed these liability shifts as necessary to controlling insurance premiums, improving the business climate, and protecting small businesses, including medical providers, from excessive litigation costs. With these arguments taking hold, it’s likely that the next phase of reform will extend beyond liability allocation into procedural barriers that reshape how malpractice claims are brought and litigated.
South Carolina’s health care sector stands to gain significantly from these reforms. Smaller practices, in particular, have long argued that under the old rules, even minimal involvement in a claim could threaten financial ruin. By narrowing the application of joint and several liability, the state has reduced one of the primary reasons insurers priced malpractice coverage so aggressively, especially for small or independent providers.
National Patterns and the Future of Malpractice Reform
While each state has taken a distinct legislative path, the common threads are unmistakable: reducing liability exposure, reshaping courtroom dynamics, and responding directly to economic and insurance pressures.
What ties these states together is their political calculus. Legislatures are no longer focusing solely on headline-grabbing caps or broad rhetorical attacks on frivolous lawsuits.
Instead, they are targeting the legal mechanics beneath the surface—what evidence juries can see, how claims can proceed, how fault is allocated, and how litigation is financed. These granular reforms deliver defense advantages long before a case reaches trial, fundamentally shifting the terrain on which malpractice battles are fought.
This wave of reform does risk overcorrecting, stacking the system so heavily in favor of defendants that legitimate malpractice victims are left without meaningful recourse. The combined effect of narrower damages, tighter procedural windows, and more limited access to litigation financing is a dangerous cocktail that erodes accountability in health care and protects institutional negligence.
What these four states illustrate is not just where malpractice law is today, but where it is headed. Future reforms are likely to push even further into procedural constraints, administrative controls, and evidence restrictions. Legislatures have learned they can bypass high-profile constitutional fights by tightening the screws at every stage of the legal process.
This is the evolving face of American tort reform—a quiet, deliberate restructuring of malpractice litigation, driven less by courtroom showdowns and more by legislative recalibration. The outcomes will ripple across health care, law, and business for years to come, shaping not only who can bring a case, but what kind of system they face when they do.