Florida stands on the edge of a sharp, decisive break from 35 years of legal precedent. With House Bill 6017 awaiting Gov. Ron DeSantis’s signature, the state is poised to repeal the so-called “free kill” law—a provision that has long barred families of unmarried adults without minor children from recovering non-economic damages in wrongful death lawsuits for medical malpractice.
If signed, the repeal will restore access to lawsuits challenging malpractice and negligence, forcing a statewide reshaping of accountability standards.
Gov. DeSantis announced on Thursday his intention to veto the long-debated bill that has been advocated by victims of medical malpractice seeking to hold health care providers accountable for alleged wrongful deaths of family members, The Orlando Sentinel reported.
Gov. DeSantis expressed concerns that repealing the law could have significant economic repercussions, specifically warning that it could lead to a sharp increase in Florida medical malpractice insurance premiums. This potential rise in costs, he argued, could negatively impact healthcare systems and providers. The debate underscores the delicate balance between ensuring access to justice for victims and maintaining stability within the medical profession.
Unpacking the Repeal—Why Now, and Why It Matters
The “free kill” provision traces back to 1990, when Florida lawmakers amended the state’s Wrongful Death Act to protect health care providers from a feared surge in malpractice lawsuits. The law barred parents of adult children over 25 and adult children of unmarried individuals from recovering non-economic damages like pain and suffering when malpractice led to death. Supporters argued this carveout was necessary to keep malpractice insurance premiums in check and prevent a mass exodus of physicians from the state.
But the savings never came.
Florida’s malpractice insurance rates have remained among the highest in the country, driven not by lawsuits but by the complexity and costs baked into the state’s health care market. Over time, the argument that this legal shield was necessary to stabilize the system began to erode. Families, left without recourse after devastating losses, turned their private grief into public pressure.
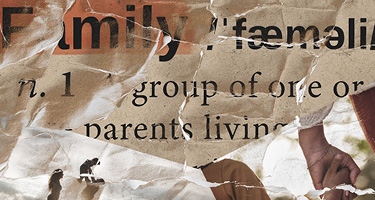
Lawmakers across party lines began to take notice. Advocates presented harrowing stories of preventable deaths and the legal dead ends families faced when the victims were unmarried adults without minor children. For many legislators, the issue became less about economics and more about fairness.
The repeal now sitting on Governor DeSantis’s desk marks a quiet but clear recalibration of Florida’s approach. If signed, it will bring the state’s wrongful death framework closer in line with national norms—restoring a right to sue that many other jurisdictions have long recognized.
This is not a dramatic expansion of liability, nor is it a wholesale shift in malpractice law. It is, simply, a correction: removing a narrow barrier that singled out certain families for exclusion.
The Corporate Fallout—What Hospitals, Insurers and Providers Face Next
For Florida’s health care providers, hospitals, and insurers, the possible repeal of the “free kill” carveout demands a thorough reassessment of institutional risk—not a panic, but a deliberate recalibration. Removing the long-standing statutory bar on wrongful death claims by certain family members expands the pool of potential plaintiffs. Even though the change looks narrow on paper, it alters how corporate actors model risk, price insurance, manage reserves, and plan long-term strategies.
At the institutional level, hospitals will need to revisit malpractice coverage limits and reassess how much financial exposure they’re willing—or able—to carry. Self-insured systems must determine whether existing reserve levels are adequate, while providers covered under broader insurance plans will see underwriters reevaluating risk profiles.
Insurers will need to adjust their models, factoring in the expanded scope of viable claims when setting future premiums. Even moderate increases in claim volume or payout size can ripple across actuarial calculations, changing how policies are priced and how risk is spread across the health care sector.
The loudest opposition to the repeal has come from medical associations and hospital executives warning of catastrophic consequences: skyrocketing insurance rates, destabilized provider networks, and the possibility that some specialties or rural hospitals will become uninsurable. But that narrative often exaggerates the immediate danger. Most structural drivers of malpractice costs—complex case mixes, defensive medicine practices, high-cost settlements, reinsurance market volatility—are only tangentially related to whether adult children or parents can bring non-economic damages claims.
A repeal is unlikely to produce the lawsuit flood some fear. Litigation volume may rise moderately, but the most likely effect is a recalibration of financial exposure, not systemic collapse.
Still, corporate risk managers cannot dismiss the shift. For decades, Florida’s providers operated under a liability environment that deliberately limited certain survivor claims.
Health care systems that refine their risk models now—before large verdicts or unexpected claim patterns emerge—will be better positioned to weather the transition. Updating reserve strategies, enhancing internal claims review processes, and working closely with insurers to ensure coverage alignment are all critical steps. For some hospitals, particularly smaller or rural providers, this may also be a moment to explore collaborative risk-pooling or alternative insurance structures to maintain financial stability.
Looking ahead, insurers and provider groups may call for new legislative safeguards to mitigate expanded liability, like lower caps on recovery. While no formal proposals have emerged, common measures in other states have included tighter pre-suit procedures, caps on non-economic damages, or limits on attorney fees.
Beyond the balance sheets, there’s an institutional reputation component at play. The repeal reflects a larger public and political sentiment shift: a demand for accountability and fair access to legal remedies. Hospitals and providers that recognize this shift and lean into transparency, patient safety initiatives, and public trust-building will not only manage their legal risk—they’ll strengthen their standing in the eyes of patients, families, and communities.
How Legal Teams Will Navigate the Shifting Landscape
While institutional actors reassess financial exposure, legal teams on both sides of the courtroom must rethink strategy, case development, and courtroom dynamics. Plaintiff lawyers will face a new task: building persuasive claims for families who were previously excluded. Adult children and parents of unmarried decedents represent a specific survivor class whose damages are inherently non-economic. These cases will turn heavily on relational evidence: the strength, depth, and day-to-day reality of the family bond.
It’s not enough to plead grief or loss in the abstract. To survive early challenges and prevail at trial, plaintiffs’ counsel will need to anchor these claims in concrete, fact-specific narratives that show jurors exactly what was taken and why it matters.
Defense attorneys must prepare for a litigation landscape where standing arguments no longer provide an early escape hatch. For decades, standing defenses helped narrow exposure and weed out claims before reaching discovery. Now, defense counsel will need to engage more deeply on the merits—focusing on causation, standard of care, and the proportionality of claimed damages. Discovery will likely expand as both sides seek detailed evidence of family dynamics, emotional impacts, and the practical consequences of the alleged malpractice.
This expansion has immediate implications for settlement negotiations. Mediations that once involved a single set of survivors and claims will increasingly include multiple claimants with different perspectives, stakes, and settlement goals. Counsel will need to manage these layered negotiations carefully, ensuring clear communication with clients and coordinated strategy across co-counsel and insurers. Ethical obligations around informed consent, client authority, and settlement allocation become even sharper in these multi-party settings.
Beyond individual cases, the repeal is likely to shape broader litigation patterns. We may see an increase in pre-trial motions challenging the sufficiency of non-economic damages evidence or seeking to limit the scope of testimony about family loss.
Courts may begin developing new case law around how to assess, cap, or apportion damages among multiple survivors. For Florida appellate practitioners, this opens a fresh area of argument and legal development—particularly as questions arise over remittitur, excessiveness, and the constitutional limits of pain and suffering awards.
Appellate courts may soon face constitutional challenges tied to the repeal—particularly around due process and proportionality when large non-economic damages awards are contested. This could open a wave of new appellate arguments, reshaping not just how malpractice cases are tried, but how damages frameworks are justified under Florida law. Litigators on both sides will need to prepare for a shifting appellate environment alongside the trial-level changes.
Importantly, malpractice attorneys—plaintiff and defense alike—will need to navigate this new terrain under heightened public scrutiny. These cases do not live solely in courtrooms. Media coverage, patient advocacy, and professional reputation all exert pressure on how claims are handled and resolved. Florida Lawyers must approach these cases with not only technical skill but strategic awareness, recognizing that the optics of fairness, accountability, and respect for survivors will shape outcomes both inside and outside the legal system.
A Measured Shift and a Lasting Impact
The possible repeal of Florida’s “free kill” law marks neither a revolution nor a collapse. It is a measured, deliberate correction—a realignment of the state’s medical malpractice system with broader principles of fairness and accountability.
For decades, the exclusion of certain survivors stood as a quiet but significant outlier in the legal landscape. Now, that carveout is poised to fall, and with it, long-standing assumptions about who gets to bring a claim and why.
The impacts will unfold over years, shaped by case law and courtroom battles. But make no mistake: Florida’s malpractice landscape is shifting, and the attorneys, judges, and institutions that move forward with clarity, preparation, and measured attention will be the ones best positioned to navigate what comes next.