In my Philadelphia office, I meet people every week who come in feeling defeated. They have paid into disability insurance for years, sometimes decades, only to be told by their insurance company that their condition is not serious enough to keep them from working. These denials are not rare. They happen to teachers, nurses, construction workers, police officers, and professionals across the city and surrounding counties.
This is not simply a story of paperwork gone wrong. It is a system designed to protect insurance companies’ bottom line. And while the denial letter can feel final, it is not the end of the road. Many claims that are initially denied can be overturned with the right evidence and persistence.
Disability in Pennsylvania: The Bigger Picture
According to the U.S. Census Bureau, more than 13 percent of Pennsylvanians live with some form of disability. Many of these individuals rely on employer-provided or private disability insurance for financial security if they can no longer work. Yet, across the state and the nation, most initial long-term disability claims are denied.
In my practice, I have represented clients from neighborhoods like Germantown, Center City, South Philly, and the Main Line. Despite differences in background, one trend is constant: insurers often issue denials first, hoping people will give up rather than appeal.
The truth is that denials are not always based on a lack of evidence. They are often part of an intentional process that places obstacles in front of claimants.
Why Insurance Companies Deny Claims
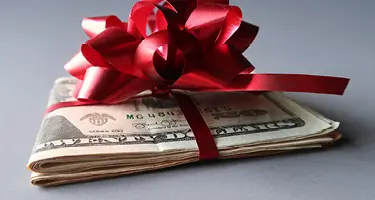
Long-term disability benefits typically pay 50 to 70 percent of a worker’s income. If someone earns $60,000 a year, an approval could mean hundreds of thousands of dollars in payments over time. Insurance companies know this. They are more motivated to deny claims than to approve them.
Common reasons for denial include claiming there is insufficient medical evidence even when a condition is well-documented; asserting the claimant can do “light” or “sedentary” work regardless of actual job availability; dismissing mental health conditions like PTSD, depression, or anxiety that are harder to measure objectively; and relying on in-house medical reviewers who conclude a person is fit to work without ever meeting them.
The pattern is the same whether the condition is a physical injury like a back disorder, or an “invisible” condition like fibromyalgia or chronic fatigue. Insurance companies frame these denials as objective decisions, but the reality is financial.
Invisible Conditions and Mental Health
One of the most frustrating realities is how insurers treat conditions that do not always show up clearly on medical tests. Fibromyalgia, lupus, multiple sclerosis, and chronic fatigue are recognized as serious, disabling conditions by medical authorities. Yet claimants often hear that their symptoms are “subjective” or “unverified.”
Mental health is another area where denials are common. For example, a police officer who develops PTSD after a traumatic event may be told by an insurer that he or she can still work, even if returning to duty would be unsafe. These decisions ignore the recommendations of treating doctors and underestimate the seriousness of the conditions.
Federal guidelines recognize both mental health disorders and chronic illnesses as legitimate bases for disability when they limit a person’s ability to function. Unfortunately, insurance companies often dismiss these diagnoses until they are challenged with strong evidence.
Understanding ERISA
Most people who receive disability insurance through an employer in Philadelphia and across Pennsylvania fall under the federal Employee Retirement Income Security Act, or ERISA. This law was meant to provide structure to employee benefits, but in practice, it makes disability appeals more difficult.
The ERISA appeal process is governed by stringent procedural rules that can be unforgiving. A claimant is typically granted only one administrative appeal, which must be filed within a 180-day window. Crucially, the entire evidentiary record must be established during this appeal; should the case later proceed to federal court, the introduction of new medical evidence is generally prohibited. Therefore, missing the appeal deadline is a final and irreversible error that almost always results in the complete forfeiture of the case.
This is one of the most important things to understand about disability denials. The clock starts ticking the moment that the denial letter arrives.
Taking Control of Your Disability Appeal
While a denial can feel overwhelming, there are proactive steps you can take to fight back effectively. From my years of experience, a successful strategy starts with demanding your complete claim file from the insurance company to scrutinize their internal reports for weaknesses. It's also vital to work with your doctors to enhance your medical records, ensuring they clearly document how your condition impairs your ability to perform your job and manage daily life. To add a personal yet powerful layer to your case, keep a detailed journal of your symptoms and limitations. Above all, you must act with urgency, as the 180-day ERISA deadline is unforgiving and missing it can terminate your claim. By taking these steps under the guidance of an experienced attorney, you can turn a seemingly hopeless denial into a successful appeal.
Why the Stakes Are So High
Many people underestimate what long-term disability benefits are worth. In addition to monthly payments replacing most of a worker’s income, benefits can continue for years or even decades. Some policies also include cost-of-living increases. In Pennsylvania, where state temporary disability coverage is limited, private or employer-sponsored long-term disability insurance can mean the difference between financial stability and bankruptcy.
Leveling the Playing Field
Insurance companies have teams of attorneys, consultants, and doctors working against claims. They know the rules inside and out. For individuals facing a denial, it can feel overwhelming to fight back alone.
That is why experience matters. After decades of representing clients across Philadelphia and Pennsylvania, I have seen the tactics insurers use. I also know the medical experts, legal procedures, and strategies that can make a case strong. Importantly, many disability lawyers, including myself, work on a contingency basis. That means no upfront legal fees. Clients only pay if their appeal is successful.
Moving Forward After a Denial
Receiving a denial letter is devastating, but it should not be the end of the fight. With proper documentation, timely appeals, and experienced legal help, many people succeed in overturning denials.
Your health condition is real, and your right to benefits is grounded in the years you paid premiums faithfully. If you are in Philadelphia or anywhere in Pennsylvania and have received a denial, do not delay. The deadlines are strict, and the evidence requirements are unforgiving.
An initial “no” from an insurance company does not have to define your future. With persistence and the right help, it is possible to secure the benefits you have earned and protect your financial security.